When you or a loved one are diagnosed with diabetic retinopathy, it's natural to feel a sense of concern about what comes next. The journey to preserve your vision in the face of this chronic disease can be complex, but understanding your treatment options is the first step towards managing your condition effectively.
Causes of Diabetic Retinopathy
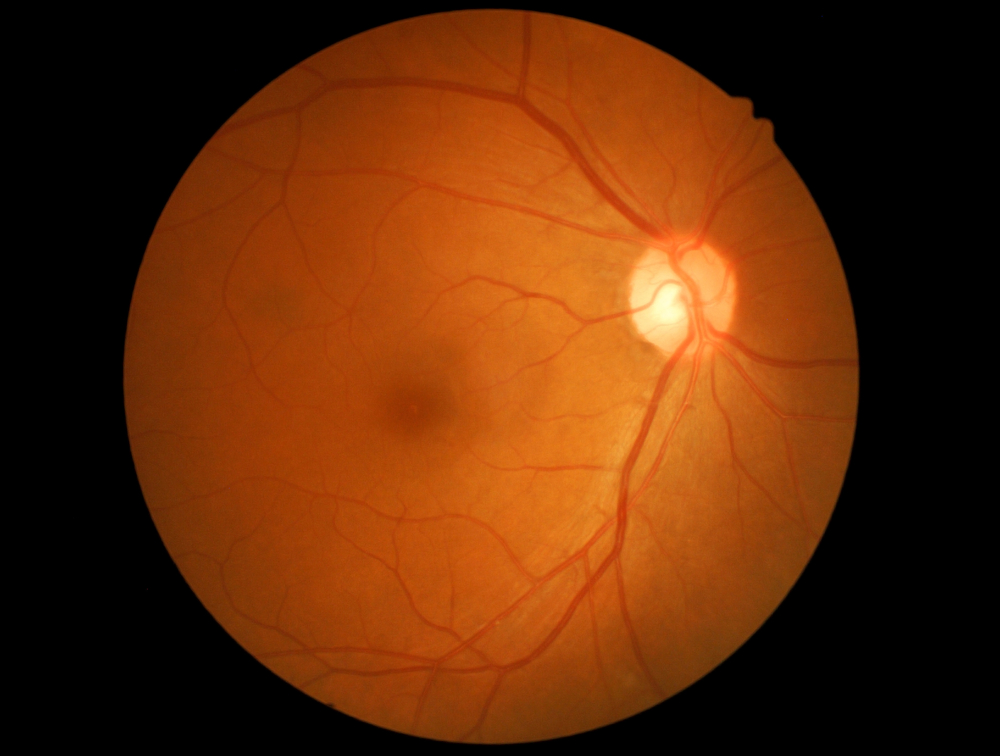
The primary cause of diabetic retinopathy is prolonged high blood sugar levels. Over time, this high glucose concentration in your bloodstream can damage the tiny blood vessels within your retina, leading to the symptoms associated with diabetic retinopathy. The likelihood of developing this condition increases the longer you have diabetes and the less controlled your blood sugar is.
Hypertension, high cholesterol, pregnancy, and tobacco use can also exacerbate diabetic retinopathy. It's imperative to manage not just your blood sugar levels but also your overall health to minimize the risk of diabetic retinopathy.
Recognizing Diabetic Retinopathy Symptoms
In the initial stages, diabetic retinopathy may not cause any noticeable symptoms. This silent progression can be deceptive, as the condition may be advancing unnoticed. As it progresses, you may start to notice symptoms such as spots or dark strings floating in your vision (floaters), blurred vision, fluctuating vision, dark or empty areas in your vision, and vision loss.
Recognizing these symptoms early is critical for timely treatment. It's recommended that if you have diabetes, you should get a comprehensive dilated eye exam at least once a year. These exams allow your ophthalmologist to detect early signs of retinal damage.
If you experience sudden vision changes or your vision becomes increasingly blurry, don't delay in seeking medical attention. Early intervention can prevent more severe complications and preserve your sight.
Treatment Options for Diabetic Retinopathy
For the ocular condition itself, non-invasive options include laser treatments and injections into the eye. Laser photocoagulation can seal leaking blood vessels or discourage new, abnormal blood vessels from forming. Injections of corticosteroids or anti-VEGF (vascular endothelial growth factor) drugs can reduce swelling of the retina and inhibit the growth of new blood vessels.
When non-invasive treatments are not sufficient, surgery may become necessary. The main surgical procedure for advanced diabetic retinopathy is called a vitrectomy. This involves removing the vitreous gel from the middle of the eye if it's filled with blood or scar tissue that's pulling on the retina. This surgery allows your ophthalmologist to access the retina and remove scar tissue, repair retinal detachment, and treat other complications.
While the thought of eye surgery can be daunting, advancements in technology have made these procedures safer and more effective. It's important to have a thorough discussion with your ophthalmologist about the potential risks and benefits of a vitrectomy or any other invasive procedure.
Navigating Diabetic Retinopathy Effectively
Diabetic retinopathy is a serious condition, but with the right knowledge and treatment plan, its progression can be managed, and your vision can be preserved. Understanding the causes and symptoms of diabetic retinopathy is key to early detection and treatment. Whether through non-invasive methods like lifestyle changes and medications, or more invasive procedures such as vitrectomy, there are several treatment options available to you.
If you're ready to learn more about your options for managing diabetic retinopathy, or if you're seeking an ophthalmologist to help guide your treatment, visit Gulf Coast Retina Center at our office in Sarasota or Venice, Florida. Be seen today or call (941) 312-2769 to schedule an appointment today.








